目次
Activities for Refreshing the Mind
Thank you for always visiting us.
This time, we will focus on “refreshing activities.”
There may not be much we can do for patients admitted to hospitals. In hospitals, treatment takes priority, and refreshing activities are often considered a luxury or secondary. I felt the same way. However, after becoming involved in home nursing care, I realized how crucial these activities are in supporting a life with illness.
Just like how we watch movies, attend concerts, or enjoy shopping to take a break from work and feel reinvigorated, patients, too, are human. Facing physical crises, they may feel encouraged or relieved by the considerate care of nurses. Since I am involved in home nursing, this is even more significant. Home care involves living with illness, requiring lifelong health considerations and facing certain inconveniences in daily life. Unlike us, they can’t freely go wherever they want or do whatever they like.
In situations where they have to ask for help to do something, they might just give up, thinking, “I don’t want to bother others.” While we can’t do everything for patients, we can offer services like massages, foot baths, listening to music, chatting, or even giving them a manicure—anything that can make them feel “That was pleasant” or “I’m happy.” Such small pleasures might help pull them out of self-deprecating thoughts like “Why did this happen to me?” or “I wish I could just disappear.”
This time, we will explore care that provides companionship and support.
1. Who Can Benefit from Refreshing Activities
For those in a hurry, please jump to the relevant sections below.
- 3. Nursing Plans
- ✩1 Elizabeth Kübler-Ross’s “Stages of Grief”
- ✩2 Patient Expectations of Physicians (1957, Reader G.G.)
- Prolonged hospitalization
- Extended stay in a facility
- Changes in the environment (adjusting to hospital life, adapting to a new routine, enduring a restricted lifestyle)
- Treatment plans (reduced immunity, restricted activity)
- Stress (from treatment, decreased activities of daily living (ADL), muscle weakness)
- Restrictions on visitation
- Separation from the mother
2. Goal Setting
In goals, the patient should be the subject.
・Anxiety and stress due to the environment or treatment are alleviated, as observed through their statements or expressions of relief.
・Stress in the therapeutic environment is reduced, and patients express comfort.
・Activities for refreshing the mind, suitable to their developmental stage, are incorporated.
・Time with family is ensured to minimize stress from being separated from them.
・A good relationship with healthcare professionals and welfare-related staff is established, allowing patients to seek advice.
3. Nursing Plans
1) Observation Plan (OP)
①Understand the patient’s current pain and anxiety:
・Physical changes due to illness, past conditions, or disabilities.
・Changes in daily living due to the above.
・Understanding of the illness and degree of self-management.
・Changes in vital signs (e.g., tachycardia, rapid breathing, high blood pressure).
・Subjective symptoms and distress (e.g., pain, palpitations, breathing difficulties, dizziness, headaches).
・Consciousness levels, delirium.
・Decreased concentration.
・Sleep disturbances.
・Depressive state.
・Pain and associated anxiety or distress.
・Anxiety about death in terminal or acute stages.
・Living in unfamiliar environments (e.g., hospital stays, facility admissions).
・Unsettling environments due to hospital smells, sounds, or voices.
・Loss of belonging (e.g., isolation from family).
・Social isolation (e.g., living away from the community due to hospitalization or admission).
・Restrictions on visits due to treatment plans (e.g., lowered immunity, special environment admissions).
・Psychiatric ward admissions.
・Long-term treatment plans (e.g., chemotherapy, radiation therapy, surgery).
・Deviation from normal processes during treatment (variance).
・Anxiety and fear of treatment, stress.
・Anxiety and fear of new environments and tasks, interpersonal discord.
Bullying.
・Environments with harassment (e.g., power harassment, sexual harassment), submissive personalities.
・Difficulty building relationships in human interactions (e.g., adaptation disorders).
・Inability to organize or express one’s thoughts or feelings.
・(Children) Interaction with parents, separation anxiety.
・(Children) Age-appropriate understanding of the purpose of hospitalization.
・(Children) Painful treatments, distressing procedures.
・(Children) Isolation from school life and friends.
・(Children) Understanding the content of treatment.
②Understand the patient’s recreation and refreshment activities:
・Patient’s hobbies, recreation.
・Trusted companions.
・Patient’s activities for refreshing the mind.
・Preferred environment, fashion.
・Patient’s personality.
2) Action Plan (TP)
・Organize the environment to ensure safety.
・Place the nurse call button within reach to prevent increased anxiety.
・Set up remote visits if visitations are restricted.
・Bring familiar items from home, like clocks or stuffed animals, for those uneasy in new environments.
・Build trust through communication and hygiene care to help patients adjust to new environments.
・Consult a doctor if sleep disturbances persist despite increased daytime activity or environmental adjustments.
・If stress arises from decreased ADL, focus on what patients can do, using assistive devices to enhance self-efficacy and alleviate dissatisfaction or anxiety.
・If anxiety or stress leads to restlessness or dangerous behavior, place the patient in a room near the nurse station for closer monitoring.
・Understand the patient’s grasp of the treatment plan and support them to stay motivated for treatment through encouragement and education.
・Conduct recreational activities for mental refreshment.
・Introduce activities for refreshing the mind (e.g., hobbies, origami, coloring, massage, reading aloud, video watching, listening, foot baths, using bath salts, walking, conversing with other patients, music, animal therapy, hospital clown performances).
・If there is anxiety about death in terminal stages, consider the stage of Kubler-Ross’s “Five Stages of Grief” and think of ways to make the remaining time meaningful, like meeting loved ones or conveying unfinished messages.
・(Children) Arrange the environment according to the child’s developmental stage, removing dangerous items and placing familiar objects.
・(Children) Provide age-appropriate preparation for treatment, avoiding false reassurances (e.g., not saying “It won’t hurt” if it will, but offering truthful support like “It will hurt, but I’ll be here with you”).
・(Children) Be mindful of language during sensitive stages like school age or adolescence, ensuring they can understand and accept their treatment according to their developmental stage.
・(Children) Include age-appropriate refreshment activities.
・(Children) Adjust visit times and locations as necessary.
✩1 Elizabeth Kübler-Ross’s “Stages of Grief”
Referenced from “Fundamentals: Psychology” by Igaku-Shoin. Kübler-Ross, an American psychiatrist, conducted interviews with 200 terminal cancer patients to investigate the psychological changes they experience before accepting death.
- Denial and Isolation: Patients cannot believe the reality of their diagnosis and may think it is a misdiagnosis or error in test data.
- Anger: Feelings of “Why me?” arise, leading to anger and resentment, often directed at family and medical staff.
- Bargaining: Patients pray to a higher power to cure them in exchange for reformed behavior.
- Depression: They begin to understand the certainty of death and may feel deep sadness or despair.
- Acceptance: Patients come to terms with their mortality, though not all reach this stage.
✩2 Patient Expectations of Physicians (1957, Reader G.G.)
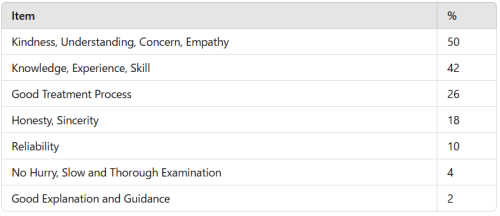
In response to the question “What do you like about your doctor?”, patients valued kindness, understanding, and empathy over technical skills or medical expertise. This sentiment applies to nurses as well, as they provide similar emotional support.
3)Educational Plan (EP)
- Discuss activities for emotional relief together with the patient.
- When patients feel down due to a decline in ADLs, focus on what they can still do and plan accordingly.
- Explore the patient’s home care environment together.
- Discuss collaboration with relevant professionals (home-visiting doctors, care managers, social workers, visiting nurses, and caregivers) after discharge.
- For financial issues related to living expenses, refer the patient to social workers or care managers.
- In cases of terminal or acute stages where fear of death is present, listen attentively and seek strategies to alleviate their anxiety, following the stages of grief.
- Explain the course of past and future treatments to those in acute stages who fear death.
- If there is pressure from superiors in the form of harassment, encourage consulting the human resources or harassment prevention department.
- In cases of bullying, suggest the patient consult with the appropriate department in the workplace.
- (For children) Work with parents to create a supportive environment and reassure the child during treatment. Ensure parents understand the treatment plan, including home care.
Thank you for reading to the end.Please feel free to leave your comments, feedback, or questions in the comment section below.

